Hamstring injuries are among the most common and frustrating injuries in sports and rehabilitation. Whether you’re an athlete, a coach, or a healthcare professional, understanding how to treat hamstring injury the right way can make the difference between a fast recovery and a chronic setback.
In this article, we’ll break down everything you need to know: what a hamstring injury is, how to assess its severity, the best treatment protocols, and how to prevent future injuries. We’ll also share key takeaways from the expert-led webinar, “Maximizing Recovery: Targeted Solutions for Hamstring Injuries” by Dr. Vien Vu, which combines scientific evidence with field-tested strategies to help you recover stronger than ever.
CONTENTS
1- What is a hamstring injury?
2- Symptoms of a hamstring injury
3- Causes and risk factors of hamstring injuries
4- Diagnosis of a hamstring injury
5- How to treat hamstring injury?
6- FAQ: Hamstring Injury Treatment & Recovery
7- Key takeaways
8- Conclusion
9- References
1- What is a hamstring injury?
Hamstring injuries are a frequent concern in sports and rehabilitation settings. They range from mild strains to complete muscle tears and can significantly impact athletic performance and daily activities. Today, the severity of these injuries is assessed based on specific grading of tissue damage, using imaging techniques (such as the Munich classification, British Athletics, etc.). Understanding the anatomy, severity levels, and early signs is key to proper treatment and prevention.
1.1. Definition
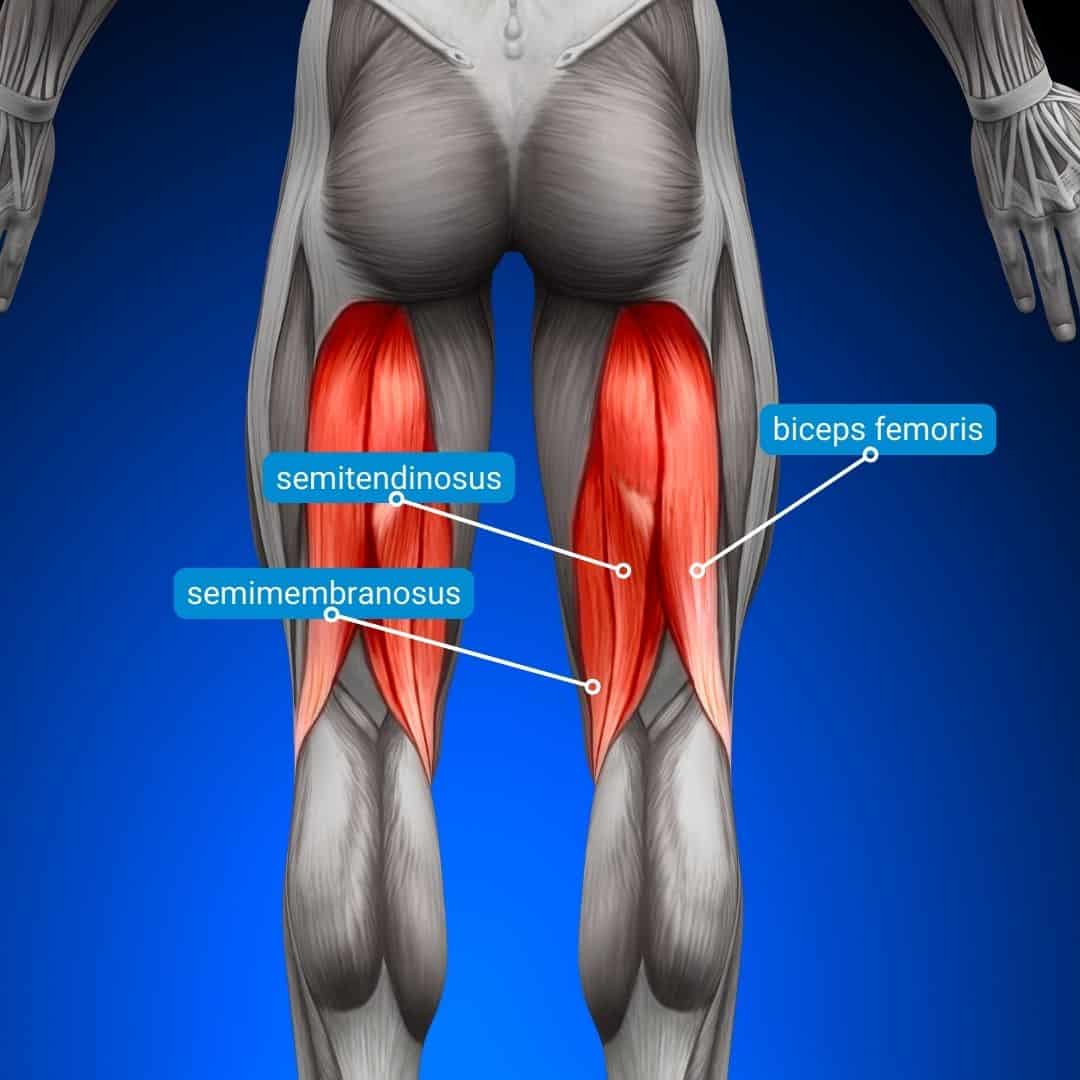
A hamstring injury refers to damage to one or more of the three muscles located at the back of your thigh: the biceps femoris, semitendinosus, and semimembranosus. These muscles work together to bend the knee and extend the hip. Injuries typically occur during activities that involve sudden acceleration, deceleration, or overstretching, like sprinting, jumping, or kicking.
1.2. The 3 grades of hamstring injuries
Hamstring injuries are categorized into three grades based on severity:
- Grade 1 (Mild strain): Minor muscle fiber damage with slight discomfort and tightness. The supporting tissue remains intact. Little or no loss of strength or mobility.
- Grade 2 (Moderate strain): Partial muscle tear, noticeable pain, swelling, reduced strength, and possible limping. There is irreversible damage to the muscle fibers and moderate involvement of the supporting tissue, often accompanied by a hematoma.
- Grade 3 (Severe tear): Complete rupture with intense pain, bruising, and significant functional impairment. There is major damage to the supporting tissue. In cases of complete tendon avulsion, it is classified as Stage 4.
Accurately identifying the grade helps guide the rehabilitation timeline and return-to-play decisions.
2- Symptoms of a hamstring injury
Recognizing the symptoms of a hamstring injury is crucial for initiating appropriate care and preventing complications. Depending on the severity, symptoms can appear suddenly or develop gradually over time.
2.1. Common signs and symptoms
- Sudden sharp pain in the back of the thigh during high-speed activities like sprinting or jumping
- Swelling or tenderness, typically within a few hours after the incident
- Bruising or skin discoloration, especially in more severe tears (Grade 2 or 3)
- Muscle weakness or difficulty bearing weight on the affected leg
- Tightness or limited range of motion in the posterior thigh
- A “popping” or snapping sensation felt at the moment of injury
Some injuries may not be immediately painful but gradually worsen with continued activity, particularly in cases of overuse.
2.2. When to see a doctor
While mild hamstring strains can often be managed with rest, ice, and self-monitoring, certain signs should prompt a professional medical evaluation:
- Inability to walk normally or bear weight on the leg
- Pain that worsens or doesn’t improve after 48-72 hours
- Visible swelling or significant bruising
- Recurring injuries in the same area
- Uncertainty about the severity or extent of the injury
💡 In the webinar Maximizing Recovery: Targeted Solutions for Hamstring Injuries, Dr. Vien Vu emphasizes the importance of involving a multidisciplinary support team early in the recovery process. A thorough clinical assessment, including strength testing and, if needed, imaging, helps avoid misdiagnosis and guides tailored rehabilitation.
About Dr Vien Vu:
Dr. Vien Vu is a Division I sports physical therapist and Associate Faculty at Tufts University’s Hybrid DPT Program. With a background in strength and conditioning, he brings a performance-first approach to rehab. He specializes in ACL recovery, healthcare disparities, and the use of technology in rehab, serving as a consultant for SimpliFaster and contributing to national research and leadership initiatives. Dr. Vu also lectures regularly on return-to-sport strategies at top U.S. universities.
3- Causes and risk factors of hamstring injuries
Understanding what causes hamstring injuries and what makes certain individuals more vulnerable is crucial for both treatment and long-term prevention. These injuries often result from a combination of mechanical stress, muscle imbalances, and external conditions.
3.1. Causes of hamstring injuries
Hamstring injuries typically occur during high-speed or explosive movements, especially when the muscle is lengthening under tension. Common causes include:
- Sudden acceleration or deceleration (for example: sprinting, jumping, or cutting)
- Overstretching the hamstring muscles during kicking or high steps
- Poor warm-up or inadequate muscle activation before intense exercise
- Fatigue, which reduces neuromuscular control and increases injury risk
- Muscle imbalances, particularly weak hamstrings compared to the quadriceps
📌 Dr. Vien Vu highlights that poor control in the terminal swing phase of running is a common moment of injury when the hamstrings contract eccentrically to decelerate the lower leg.
3.2. Risk factors
Certain intrinsic and extrinsic factors increase the likelihood of hamstring injury:
- Previous hamstring injury – the single most significant risk factor
- Age – older athletes are more susceptible
- Lack of flexibility or strength, especially eccentric strength
- Poor lumbopelvic control, affecting hip and trunk mechanics
- High-speed sports participation (for example: football, rugby, track)
- Training errors, like sudden increases in intensity or volume
As emphasized in the webinar, a history of previous hamstring injury increases the risk of recurrence threefold. This underlines the need for personalized rehab plans and objective return-to-play criteria.
4- Diagnosis of a hamstring injury
Accurate diagnosis is the foundation of effective treatment. It helps determine the grade of the injury, guides clinical decision-making, and influences return-to-play timelines.
A proper diagnosis of a hamstring injury combines clinical evaluation, functional testing, and, when necessary, imaging.
4.1. Clinical assessment
The first step involves a thorough clinical examination:
- Patient history (onset, mechanism of injury, previous injuries): It is essential to consider injury history when assessing athletes. Dr. Vien Vu cites a study showing that athletes with a history of hamstring injuries are three times more likely to get injured again. This finding suggests that professionals must be especially vigilant during the rehabilitation of these athletes and tailor their protocols accordingly.
- Palpation to locate pain and assess swelling
- Range of motion (ROM) and strength testing, particularly for hip extension and knee flexion
- Gait analysis and functional tests (for example, single-leg tasks, hop tests)
A key takeaway from the webinar is the importance of objective testing, as emphasized by Dr. Vien Vu. He recommends eccentric strength tests and isokinetic dynamometry to detect subtle deficits that may go unnoticed in basic evaluations.
4.2. Imaging: When and why
Imaging is not always necessary, but can help in certain cases:
- MRI (Magnetic Resonance Imaging) is useful to assess the extent of muscle tearing, hematomas, and tendon involvement.
- Ultrasound can be used for real-time dynamic imaging, especially in acute cases.
However, Dr. Vu cautions against over-reliance on imaging. He points out that 21% of severe hamstring injuries may show no structural damage on MRI, reinforcing the need for comprehensive clinical judgment.
4.3. The role of objective metrics
Integrating technology into the diagnostic process enhances precision. Solutions like the Kinvent dynamometers allow clinicians to:
- Quantify knee flexor strength
- Track asymmetries between limbs
- Monitor progress during rehab
Using objective metrics aligns with evidence-based guidelines and helps tailor rehabilitation programs to the athlete’s specific needs, reducing the risk of reinjury.
5- How to treat hamstring injury?
Effective treatment of a hamstring injury involves a progressive, evidence-based approach that balances rest, active rehabilitation, and objective evaluation. While mild strains may resolve with basic care, more severe or recurrent injuries require a structured rehab plan.
5.1. Initial management: The acute phase
In the first 48-72 hours following injury, the focus is on protecting the muscle from further damage and reducing inflammation:
- Relative rest (avoid high-speed or painful activity)
- Ice application to reduce pain and swelling
- Compression and elevation to manage inflammation
- Gentle mobility exercises as tolerated
Complete immobilization is discouraged, as early mobilization improves long-term outcomes. Pain-free movement should begin as soon as possible.
5.2. Progressive rehabilitation
As symptoms subside, treatment should evolve toward active recovery:
- Stretching and range of motion exercises
- Progressive strengthening, starting with isometrics → concentric → eccentric
- Neuromuscular control training to address coordination and stability
- Sport-specific drills to prepare for return to performance
Dr. Vien Vu, in the webinar, advocates for rehabilitation based on individual deficits rather than generic protocols. He compares two rehabilitation protocols: a generalized program and one based on individual deficits. The results show that those following a deficit-based program have a six times lower risk of reinjury. This indicates that personalized approaches, which take into account the specific needs of each athlete, are more effective in the rehabilitation process.
5.3. Use of objective tools and technology
To tailor and monitor rehab effectively, Dr. Vu recommends integrating objective testing tools, such as:
- Isokinetic testing to evaluate hamstring torque at different speeds
- Handheld or connected dynamometers and goniometers (for example, Kinvent K-Push, K-Pull, and K-Move) to quantify strength gains
- Functional tests like the Nordic hamstring tests, or single-leg bridge holds
These tools help ensure that strength asymmetries and neuromuscular deficits are addressed before returning to sport.
💡Tutorial: How to evaluate your hamstring strength using the K-Push:
5.4. Team-based approach
Dr. Vu strongly emphasizes interdisciplinary collaboration in the treatment process. This includes:
- Physical therapists for rehab progression
- Strength and conditioning coaches for reintegration to training
- Physicians or sports medicine specialists for ongoing evaluation
- Athlete education to ensure understanding and adherence
This collaborative model supports a holistic and athlete-centered recovery plan, significantly improving outcomes and reducing recurrence.
6- FAQ: Hamstring Injury Treatment & Recovery
Is walking good for hamstring pain?
It depends on the severity of the injury. For mild strains (Grade I), gentle walking can promote blood flow and healing. However, if pain persists or worsens during walking, rest is essential. Avoid limping, as it can lead to compensatory injuries.
How long does it take for a hamstring injury to heal?
Healing time varies:
- Grade I (mild strain): 1–2 weeks
- Grade II (partial tear): 3–6 weeks
- Grade III (complete tear): several months and may require surgery
Rehabilitation progress should be guided by objective measures, not just pain resolution.
Rehabilitation progress should be guided by objective measurements, not just by the disappearance of pain.
Is heat good for a pulled hamstring?
Heat can help reduce muscle tension and improve circulation during the later stages of recovery. However, avoid heat in the acute phase (first 48–72 hours) when inflammation is present. Cold therapy is recommended early on.
How to treat a hamstring injury at home?
In the early phase:
- Rest the muscle and avoid aggravating activities
- Ice the area for 15–20 minutes every few hours.
- Compression with an elastic bandage can reduce swelling.
- Elevation helps drainage
After a few days, gentle stretching and isometric exercises may be introduced if pain allows. However, for complete recovery, consult a healthcare professional.
Should I stretch a pulled hamstring?
Not immediately. Stretching a recently injured muscle can worsen the damage. Wait until the acute pain and inflammation subside. Then, progress gradually with controlled stretches under professional guidance. Focus on flexibility only once the strength is restored.
7- Key takeaways
Hamstring injuries, though common, require a nuanced and individualized approach for optimal recovery. Accurately identifying the severity of the injury, whether it’s a mild strain or a complete tear, is essential, as it directly impacts the rehabilitation timeline and return-to-play decisions.
A number of risk factors contribute to these injuries, including previous strains, inadequate eccentric strength, neuromuscular imbalances, and poor control during the terminal swing phase of sprinting.
Effective diagnosis hinges on combining clinical evaluation with functional testing and, when appropriate, imaging. However, as Dr. Vien Vu emphasizes in the webinar, imaging alone is not sufficient; objective strength and performance assessments are crucial. Technology like isokinetic dynamometers and connected sensors, such as Kinvent’s K-Push or K-Pull, allows clinicians to quantify deficits and track real progress throughout recovery.
Treatment should avoid complete rest and instead promote early, pain-free mobility. As symptoms improve, rehabilitation must be progressive, shifting from isometric to eccentric work and integrating coordination, stability, and sport-specific drills. Importantly, rehabilitation should not follow a generic timeline, but rather be tailored to the athlete’s specific deficits. This approach has been shown to significantly reduce reinjury rates.
Finally, a multidisciplinary and collaborative approach is key to successful recovery. Physical therapists, strength and conditioning coaches, physicians, and the athlete themselves should work together to build a comprehensive, objective, and performance-oriented rehab plan.
8- Conclusion
Recovering from a hamstring injury isn’t just about healing. It’s about returning stronger, smarter, and more resilient. With the right strategy in place, starting from an accurate diagnosis, through tailored rehab and objective monitoring, athletes can avoid chronic setbacks and significantly reduce their risk of reinjury.
As Dr. Vien Vu’s insights demonstrate, combining scientific evidence with practical sensors and a team-based approach offers the best path to recovery. Whether you’re a healthcare provider, a coach, or an athlete, mastering the principles of targeted hamstring rehab is essential for long-term performance and safety.
9- References
- Wangensteen et al., Hamstring Reinjuries Occur at the Same Location and Early After Return to Sport, 2016.
- Schneider‑Kolsky et al., A comparison between clinical assessment and magnetic resonance imaging of acute hamstring injuries, 2006.
- Torres‑Velazquez et al., MRI Radiomics for Hamstring Strain Injury Identification and Return to Sport Classification, 2024.
- Martin et al., Hamstring Strain Injury in Athletes, 2022.