Chronic Obstructive Pulmonary Disease (COPD) is far more than just a lung condition. Over the years, research has revealed its widespread impact, especially on peripheral muscles.
Loss of strength, muscle wasting, and reduced endurance are common yet often overlooked consequences. These factors significantly affect patients’ functional independence and worsen long-term outcomes.
Despite this, muscle strength assessment remains underused in clinical practice. In this article, we explore why evaluating muscle strength in COPD patients is now essential, what tools are most effective, and how these data can help transform respiratory rehabilitation strategies.
CONTENTS:
1- COPD and Muscle Weakness: An Underestimated Clinical Issue
2- Quadriceps and Grip Strength: Key Clinical Indicators
3- The Most Reliable Strength Tests in Clinical Practice
4- Overcoming Barriers to Muscle Strength Assessment
5- Patient Monitoring: Why Quantification Changes Everything
6- Key Takeaways
7- FAQ: Muscle Strength Testing in COPD Rehab
8- Conclusion
9- References
1- COPD and Muscle Weakness: An Underestimated Clinical Issue
In patients with COPD, peripheral muscle dysfunction is common, yet still largely underdiagnosed. And its clinical impact is anything but minor.
Chronic dyspnea, systemic inflammation, corticosteroid use, and especially the sedentary lifestyle associated with COPD all contribute to progressive muscle wasting, particularly in the lower limbs. The quadriceps femoris is among the first muscles affected. This loss of strength has direct consequences: reduced walking ability, difficulty climbing stairs, and increased dependence in daily life.
Several studies have highlighted the scope of the problem:
- According to Shrikrishna et al. (2012), physical inactivity in COPD patients is strongly linked to quadriceps atrophy, fueling a downward spiral of deconditioning and functional decline.
- Shah et al. (2019) quantified an average 28% reduction in quadriceps strength in COPD patients compared to healthy individuals of the same age.
In other words, muscle weakness isn’t a late-stage complication; it’s an early, modifiable marker of disease progression. That’s why routine muscle strength assessment should be a core part of COPD management.
2- Quadriceps and Grip Strength: Key Clinical Indicators
In COPD patients, muscle weakness, especially in the quadriceps and hands, isn’t just another symptom. It’s a major clinical marker.
Quadriceps Strength: A Powerful Prognostic Tool
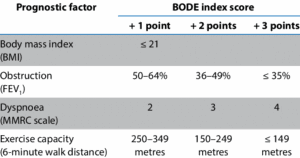
Beyond its obvious role in movement, quadriceps strength is directly linked to mortality risk and disease progression in COPD. According to Shrikrishna et al. (2012), it serves as a strong predictor and is one of the key elements of the BODE index, which combines BMI, airflow obstruction, dyspnea, and exercise capacity to estimate survival risk.
💡 What is the BODE Index? The BODE Index is a multidimensional tool used to assess the risk of exacerbations and mortality in people with COPD. It also helps clinicians determine disease severity based on FEV1 and walking distance. However, some of its components can be hard to measure or require specific equipment.
Recent guidelines emphasize the importance of assessing quadriceps strength to:
- Detect early and severe deconditioning,
- Set personalized rehabilitation goals,
- Monitor the effects of therapeutic interventions over time.
Grip Strength: A Simple, Yet Powerful Metric
Less common in respiratory rehab but gaining ground, grip strength is now recognized as a global marker of muscle strength and overall health. Research shows it’s linked to:
- Sarcopenia risk,
- Cardiovascular morbidity,
- And even mortality, including among COPD patients (Jeong et al., 2017).
Its ease of use makes it a valuable screening tool, even during regular consultations or home visits.
3- The Most Reliable Strength Tests in Clinical Practice
Muscle strength testing is no longer limited to research labs or hospital settings. Today, quick, validated, and reproducible assessments can be performed directly in outpatient clinics in just a few minutes.
Quadriceps Strength Test: A Respiratory Rehab Essential
One of the most commonly used tests in pulmonary rehabilitation is the isometric quadriceps strength test. The patient pushes against a fixed resistance without joint movement. The ideal setup involves a portable dynamometer placed at the ankle while the patient is seated with knees bent at 90°.
This test offers multiple clinical advantages:
- High reliability, even across different practitioners,
- Sensitivity to change, making it ideal for tracking progress over time,
- Safe and low-fatigue, suitable even for frail or severely deconditioned patients.
Reference values based on age, gender, and clinical condition help interpret the results with precision. This makes the test especially valuable when performed with digital dynamometers, which are considered the gold standard for measuring muscle strength and power (Shrikrishna et al., 2012).

💡 The traction dynamometer K-Pull, a connected and portable traction dynamometer, is perfectly suited for this test. Attached to the ankle or a fixed point, it accurately measures isometric quadriceps strength. When paired with the Kinvent App, it delivers instant data, tracks progress objectively, and integrates smoothly into patient assessments.
Handgrip Dynamometry: A Fast and Reliable Strength Marker
Even easier to perform than the quadriceps test, the handgrip test measures the maximum grip strength of the dominant hand using a handheld dynamometer. This assessment offers several key benefits:
- Extremely quick (just a few seconds),
- Non-invasive,
- Suitable for all patients, including those who are severely deconditioned.
It’s especially useful as a first-line screening tool for detecting global muscle weakness or as a complementary measure to quadriceps testing. It can also help diagnose sarcopenia based on the criteria from the European Working Group on Sarcopenia in Older People (EWGSOP).
According to Saey et al. (2021), digital dynamometry is now the gold standard for assessing muscle function, whether evaluating lower limb strength (quadriceps) or grip strength.

💡 The grip dynamometer K-Grip fits seamlessly into this approach. This connected, accurate, and portable device delivers fast and reliable grip strength measurements.
Paired with the Kinvent app, it offers:
- Automated data tracking,
- Real-time progress visualization,
- And easy export of clinical reports, saving valuable time for healthcare professionals.
4- Overcoming Barriers to Muscle Strength Assessment
Despite their proven value, muscle strength assessments remain underused in outpatient pulmonary rehabilitation. Why? Several barriers exist, but most are easily overcome.
Barrier #1: “I don’t have the right equipment.”
Muscle testing was once associated with bulky, hospital-grade devices. Today, portable and accurate dynamometers are available at accessible prices. Coupled with digital apps, they simplify data interpretation and patient follow-up.
Barrier #2: “I don’t have time during sessions.”
We get it! Sessions are short, and priorities are many. But here’s the good news:
- The grip strength test takes less than one minute,
- The isometric quadriceps test can be integrated into a standard strength session,
- And digital tools automate analysis and reporting, saving you time.
Muscle testing can fit naturally into your clinical routine without adding complexity to patient care.
Barrier #3: “I don’t know how to interpret the results.”
Helpful resources are readily available:
- Normative reference charts,
- Validated clinical thresholds,
- And even training modules.
With simple tools, you can detect clinically relevant muscle weakness, monitor progression, and decide when to reassess.
5- Patient Monitoring: Why Quantification Changes Everything
Measuring muscle strength once is helpful. But tracking it over time is where the real clinical impact lies. For patients with COPD, quantification brings powerful value to rehabilitation strategies.
Turning Progress Into Data
Without measurable outcomes, it’s hard to know whether a protocol is truly working. By quantifying performance (for example, +15% quadriceps strength after 6 weeks), physical therapists can:
- Adjust training intensity,
- Reassess goals when needed,
- And communicate more clearly with patients and referring physicians.
It also helps identify early signs of stagnation or decline, even when follow-up is ongoing.
Boosting Patient Motivation
Seeing progress in real numbers is a powerful motivator, especially in chronic conditions like COPD, where long-term commitment can fade. Quantified improvements turn abstract gains into concrete benefits: “Before, I couldn’t get up without using my arms. Now I’m pushing stronger than when I started!”
Creating a Shared Language Across Providers
Objective data facilitates communication with prescribers, physicians, or other physiotherapists involved in the patient’s care. It improves continuity and highlights the value of physical therapy in managing severe respiratory diseases.
💡 With digital tools like the Kinvent app, all strength tests performed using Kinvent sensors (e.g., K-Pull or K-Grip) are:
- Automatically recorded,
- Saved in the patient’s history,
- And displayed in clear, visual charts.
These numerical insights have real clinical power. They help:
- Identify high-risk patients likely to worsen or experience COPD exacerbations,
- Act early with lifestyle or therapeutic adjustments (European Respiratory Journal, 2012),
- And build individualized training programs based on actual capacity.
For the physical therapist, this translates into time savings and improved traceability: assessments are exportable, progress curves are accessible in seconds, and patient engagement is enhanced through clear, session-by-session tracking. The My Kinvent feature extends this follow-up beyond the clinic by giving both patients and referring physicians secure access to test results and data. It also facilitates communication by allowing:
- appointment scheduling,
- the sending of questionnaires and Patient-Reported Outcome Measures (PROMs),
- and seamless sharing of clinical information.
All of this is done in a GDPR-compliant environment, ensuring the protection of each user’s health data.
6- Key Takeaways
- COPD is often accompanied by major peripheral muscle weakness, especially in the quadriceps and grip strength.
- These muscle indicators are closely linked to mortality risk, sarcopenia, inactivity, and the functional progression of the disease.
- Simple, validated tests can be performed in-clinic to assess muscle strength: isometric dynamometry for quadriceps and handgrip.
- Common barriers to strength testing such as lack of equipment, time, or reference values can be overcome with modern, portable tools that are easy to use and interpret.
- The Kinvent app provides a fast, visual, and fully digitalized workflow that boosts patient adherence and supports better clinical decisions.
- Tracking muscle strength over time helps to objectify progress, personalize rehabilitation protocols, and improve multidisciplinary coordination.
7- FAQ: Muscle Strength Testing in COPD Rehab
What are the best strength tests for respiratory rehabilitation?
The most relevant ones are:
- Isometric quadriceps strength test (performed seated or lying down, with a dynamometer),
- Handgrip strength test, using a handheld dynamometer.
These tests are simple, quick to perform, and validated in clinical research.
How often should muscle strength be assessed?
Ideally, at the start of the rehab program, then every 4 to 6 weeks, to adjust goals. For long-term follow-up, a quarterly evaluation helps track improvement or stability.
Is a manual dynamometer enough?
Yes. As long as it’s reliable and properly calibrated. However, digital dynamometers (like those from Kinvent) offer the advantage of automated tracking and real-time visual feedback through a dedicated app.
Why is handgrip strength relevant for COPD patients?
Grip strength is a global marker of muscle health. It’s correlated with sarcopenia, fall risk, cardiovascular complications, and even mortality in various studies. In COPD, it provides a fast and valuable clinical indicator.
Do patients respond well to these tests?
Absolutely. Most patients appreciate seeing their progress over time. The tests are well-tolerated, even by frail individuals, and contribute to stronger engagement in the rehabilitation process.
8- Conclusion
In the context of COPD, assessing muscle strength is no longer a “nice to have”; it’s a clinical necessity. Weakness in the quadriceps or reduced grip strength isn’t just a peripheral symptom: it’s a key indicator of functional status, complication risk, and overall prognosis.
The good news? These parameters can now be measured easily and efficiently in-clinic, using simple, portable, scientifically validated, and connected tools. The Kinvent app, paired with Kinvent sensors, streamlines this process and saves valuable clinical time.
Bringing strength quantification back into your assessments and follow-ups means gaining a clearer picture of patient needs, delivering more personalized care, and demonstrating the real impact of your rehabilitation practice.
9- References
- HAS : Comment mettre en œuvre la réhabilitation respiratoire pour les patients ayant une bronchopneumopathie chronique obstructive ?
- Saey D, Bellocq A, Gephine S, Lino A, Reychler G, Villiot-Danger E. Quels tests physiques pour quels objectifs en réadaptation respiratoire ? Revue des Maladies Respiratoires. 1 juin 2021 ;38(6) :646–63.
- Ramalho SHR. Lung function and cardiovascular disease: a link. Trends Cardiovasc Med. 2021.
- La Réadaptation Cardiaque – Phase 2, FÉDÉRATION FRANÇAISE DE CARDIOLOGIE
- Houssière A. L’index BODE : révélateur de l’intérêt de l’évaluation de la dysfonction musculaire chez le BPCO. 2010.
- Hamilton AC. Muscle strength, symptom intensity, and exercise capacity in patients with cardiorespiratory disorders. Am J Respir Crit care Med. 1995.
- Maltais F. Dysfonction musculaire périphérique dans la BPCO. Rev Mal Respir. 2022.
- Shah S, Darekar B, Salvi S, Kowale A. Quadriceps strength in patients with chronic obstructive pulmonary disease. Lung India. oct 2019;36(5):417–21.
- Shrikrishna D, Patel M, Tanner RJ, Seymour JM, Connolly BA, Puthucheary ZA, et al. Quadriceps wasting and physical inactivity in patients with COPD. European Respiratory Journal. 1 nov 2012;40(5):1115–22.
- Jeong M, Kang HK, Song P, Park HK, Jung H, Lee SS, et al. Hand grip strength in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2017;12:2385–90.
- Holland A. The BODE Index. Journal of Physiotherapy. 1 janv 2010;56(1):62.


